Can Diabetic Retinopathy Be Reversed? Symptoms, Treatment & Prevention
Diabetic retinopathy cannot be fully reversed, but early-stage cases can be managed to slow or stop progression. Maintaining healthy blood sugar levels and making lifestyle changes can help preserve vision. Advanced stages often require medical intervention to prevent further damage and vision loss.
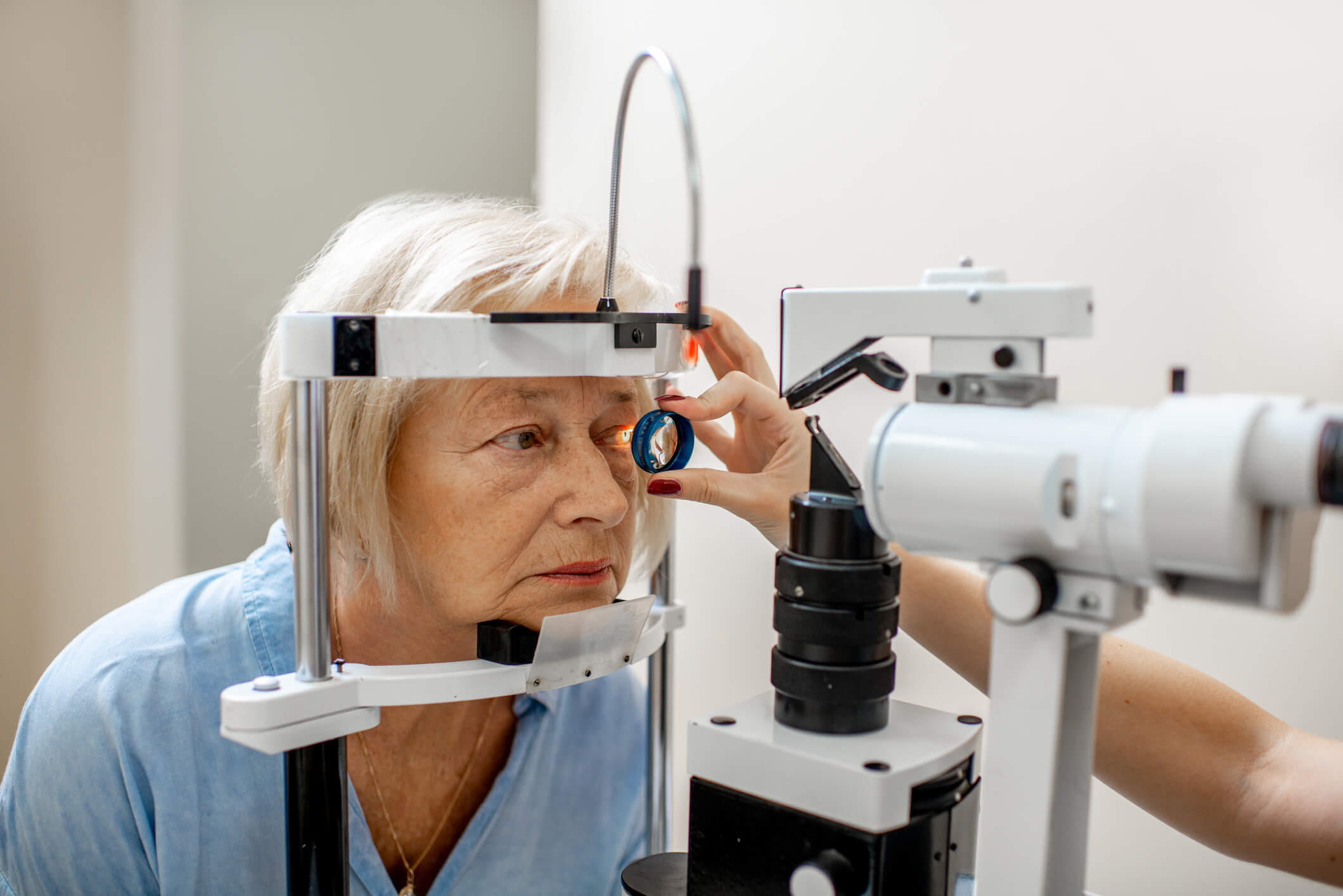
Many people with diabetes don’t experience noticeable symptoms until the condition has already caused retinal damage. That’s why regular eye exams are essential – they can detect changes in the tiny blood vessels of the retina before significant vision problems occur.
More About Diabetic Retinopathy
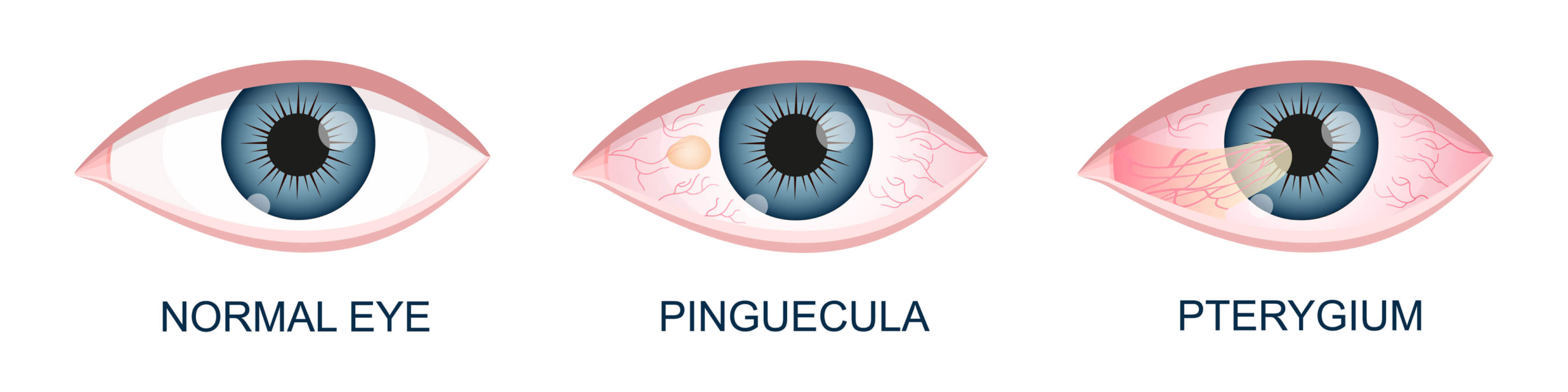
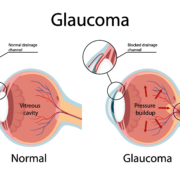
Diabetic retinopathy develops when high blood sugar levels damage the blood vessels in the retina, the light-sensitive tissue at the back of the eye. Over time, these blood vessels can leak fluid, become blocked, or lead to the growth of abnormal blood vessels, all of which can cause vision problems.
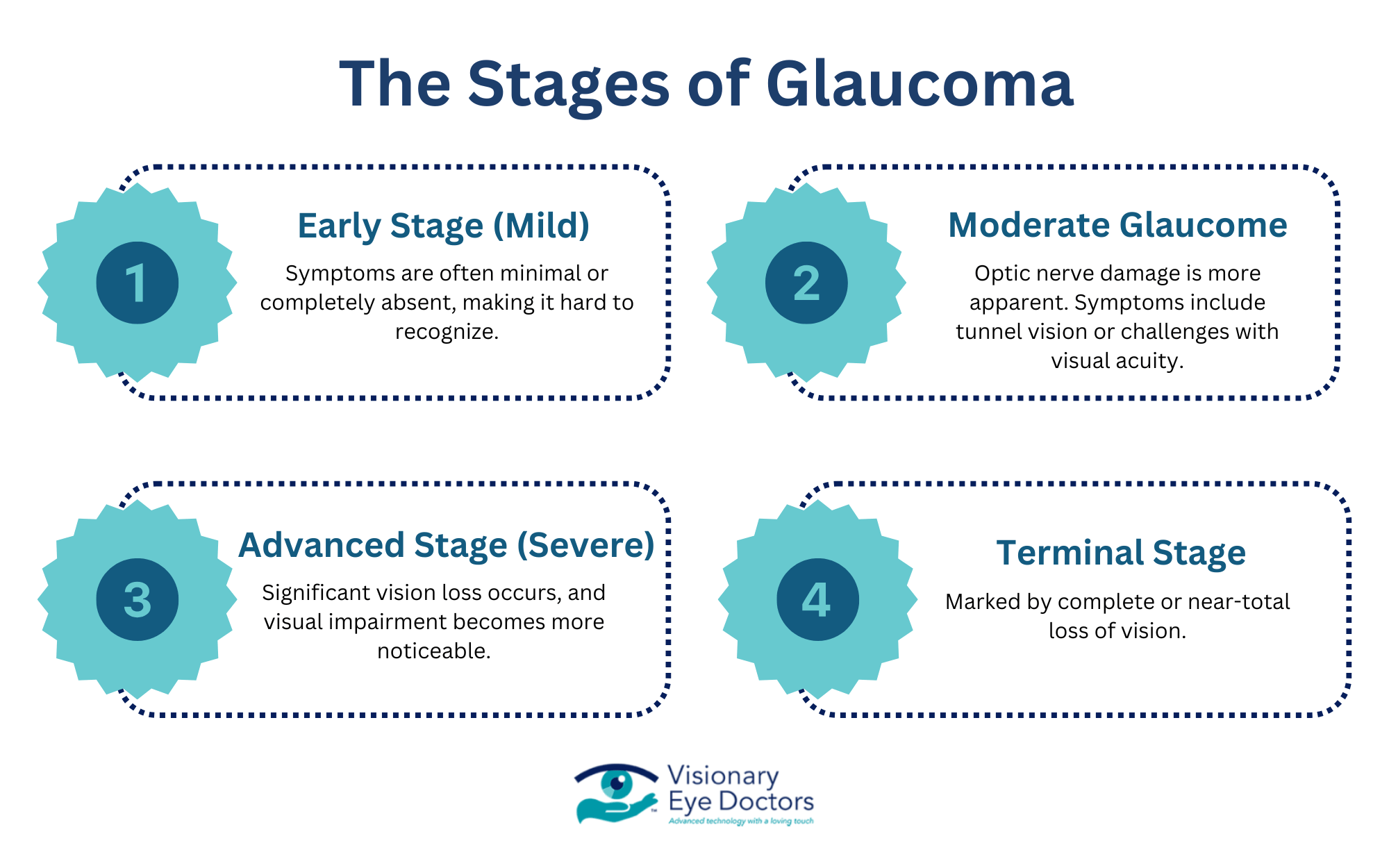
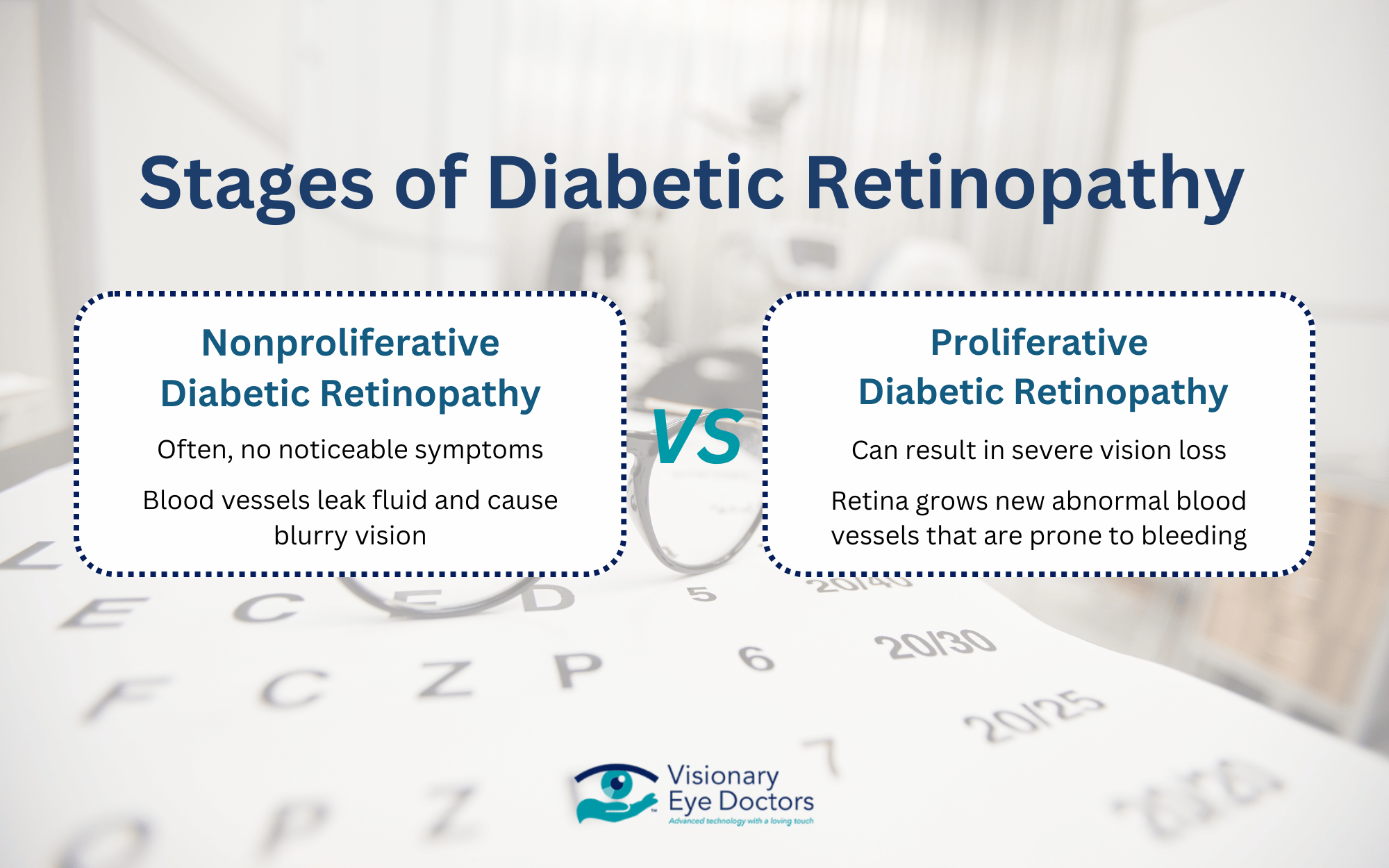
Stages of Diabetic Retinopathy
- Nonproliferative Diabetic Retinopathy
-
-
- Blood vessels leak fluid, leading to diabetic macular edema that causes blurry vision
- Many people have no symptoms at this early stage
-
- Proliferative Diabetic Retinopathy
-
- The retina tries to compensate by growing new blood vessels, but these are fragile and prone to bleeding and scarring
- Without treatment, this can result in severe vision loss
Managing blood sugar, blood pressure, and cholesterol levels can help slow the progression and protect your vision. Regular eye exams allow for early detection and intervention before significant damage occurs.
Signs and Symptoms
Diabetic retinopathy progresses gradually, with early symptoms including:
- Blurry vision that fluctuates
- Floaters (dark spots or strings in your vision)
- Difficulty seeing at night or adjusting to dim light
- Distorted vision, where straight lines appear wavy
- Dark or empty areas in vision
- Sudden vision loss (in severe cases)
Is Diabetic Retinopathy Reversible?
Once retinal blood vessels are damaged, the effects are often permanent, particularly in advanced cases where abnormal blood vessels grow or scar tissue forms. However, early intervention can significantly reduce the risk of vision loss and prevent further damage.
Early Stage vs. Advanced Stage
At the early stages of nonproliferative diabetic retinopathy, the focus is on preventing progression through controlling blood sugar, blood pressure, and cholesterol.
When caught early, diabetic retinopathy may not require immediate medical treatment but does require regular eye exams to monitor changes.
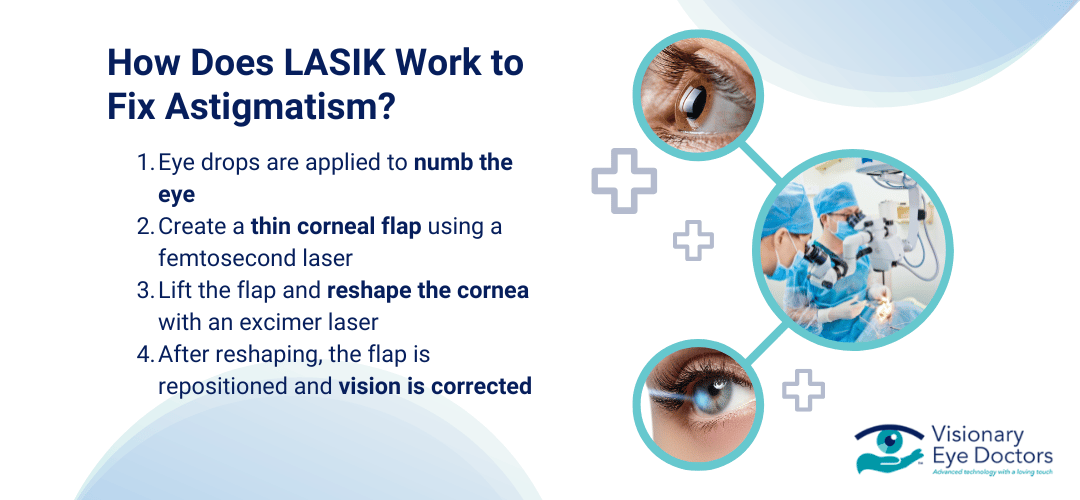
In advanced proliferative diabetic retinopathy, blood vessels are abnormal and fragile. At this stage, medical treatment is necessary to prevent permanent vision loss. Treatment methods can include laser therapy, anti-VEGF injections, and vitrectomy surgery.
The Role of Lifestyle Changes in Managing Diabetic Retinopathy
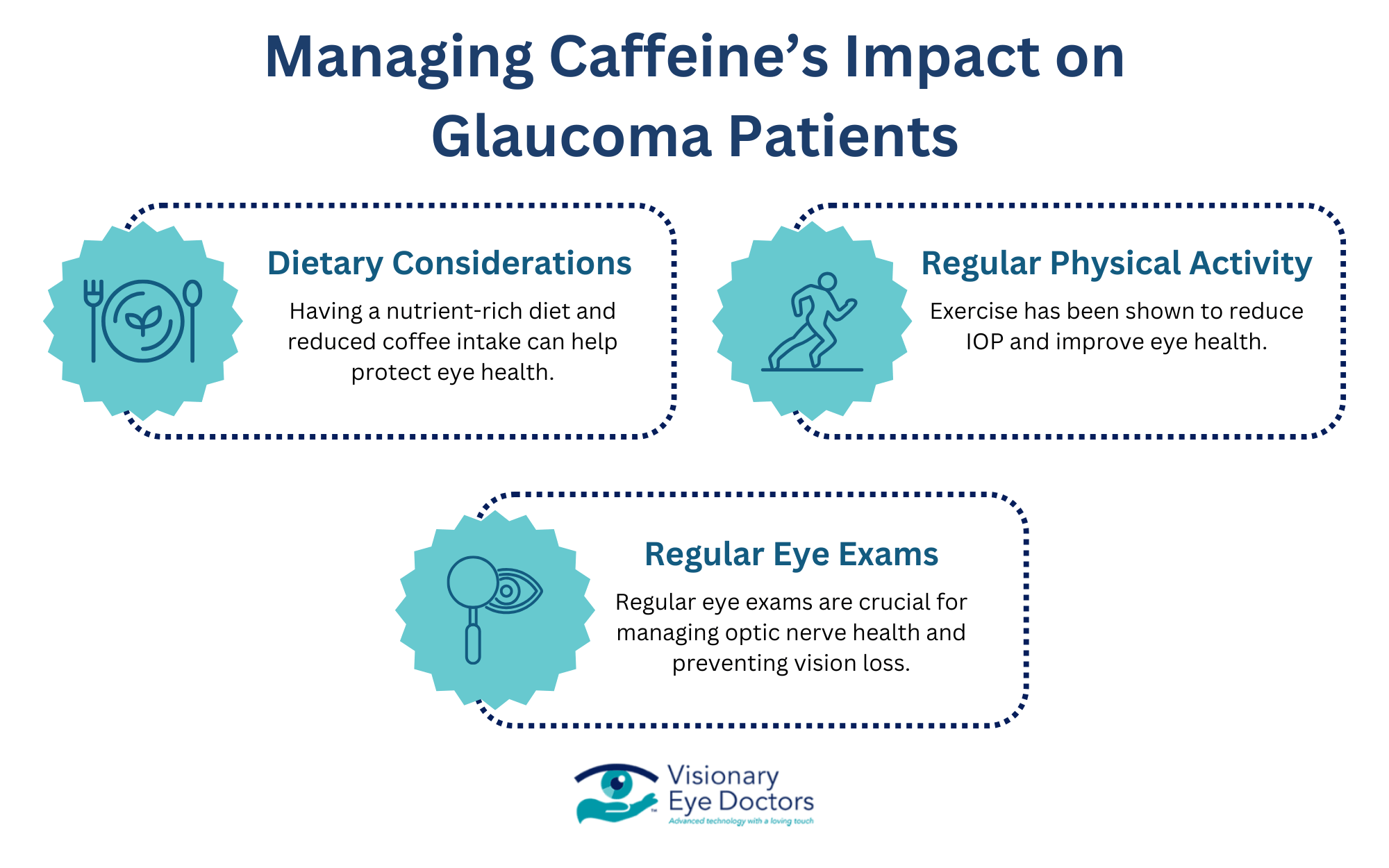
While medical treatments target existing damage, lifestyle changes help prevent worsening symptoms and protect long-term vision health.
- Blood sugar control reduces the stress of retinal blood vessels
- Lowering blood pressure and cholesterol prevents further harm to the tiny blood vessels in the eye
- Regular exercise improves blood flow
- Antioxidants and omega-3s help limit oxidative stress, which contributes to retinal damage
The Importance of Regular Eye Exams
Because diabetic retinopathy often develops without noticeable symptoms, routine eye exams are essential. Tests like optical coherence tomography (OCT) allow an eye doctor to detect subtle changes in the retina before vision problems appear.
Although this eye condition cannot be reversed, early intervention and consistent management can help preserve vision and prevent severe complications.
In-Depth Treatment Options for Diabetic Retinopathy
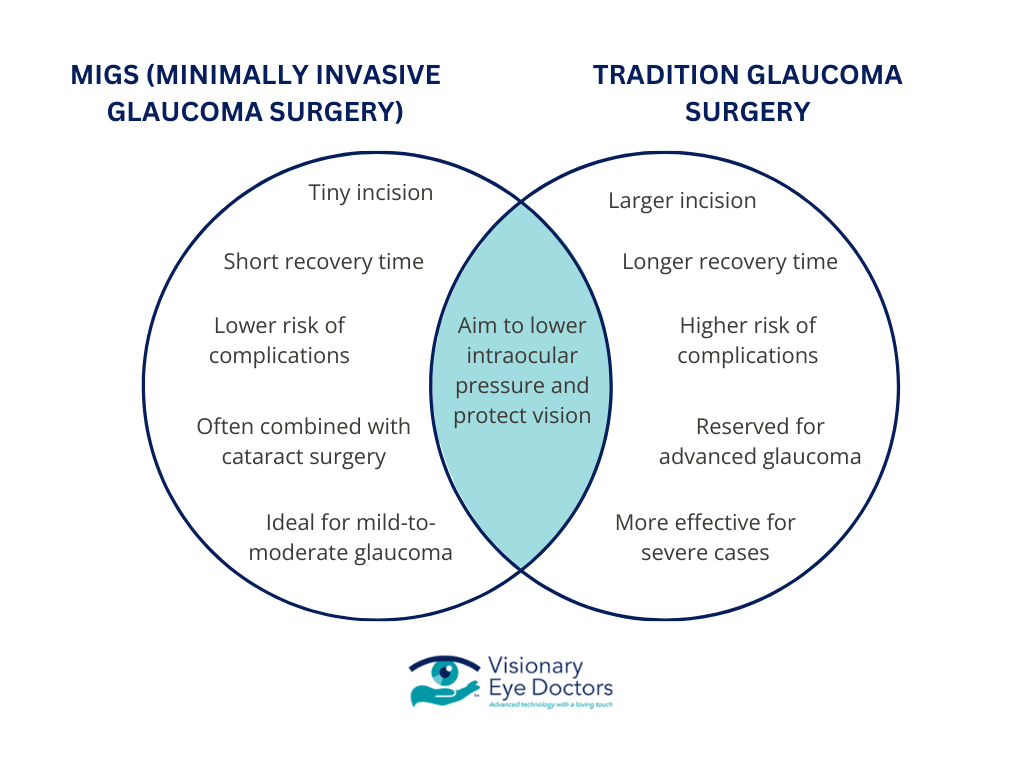
While diabetic retinopathy cannot be reversed, several treatments can slow its progression and prevent vision loss. The right approach depends on the severity of the condition and whether diabetic macular edema (DME) or proliferative diabetic retinopathy (PDR) is present.
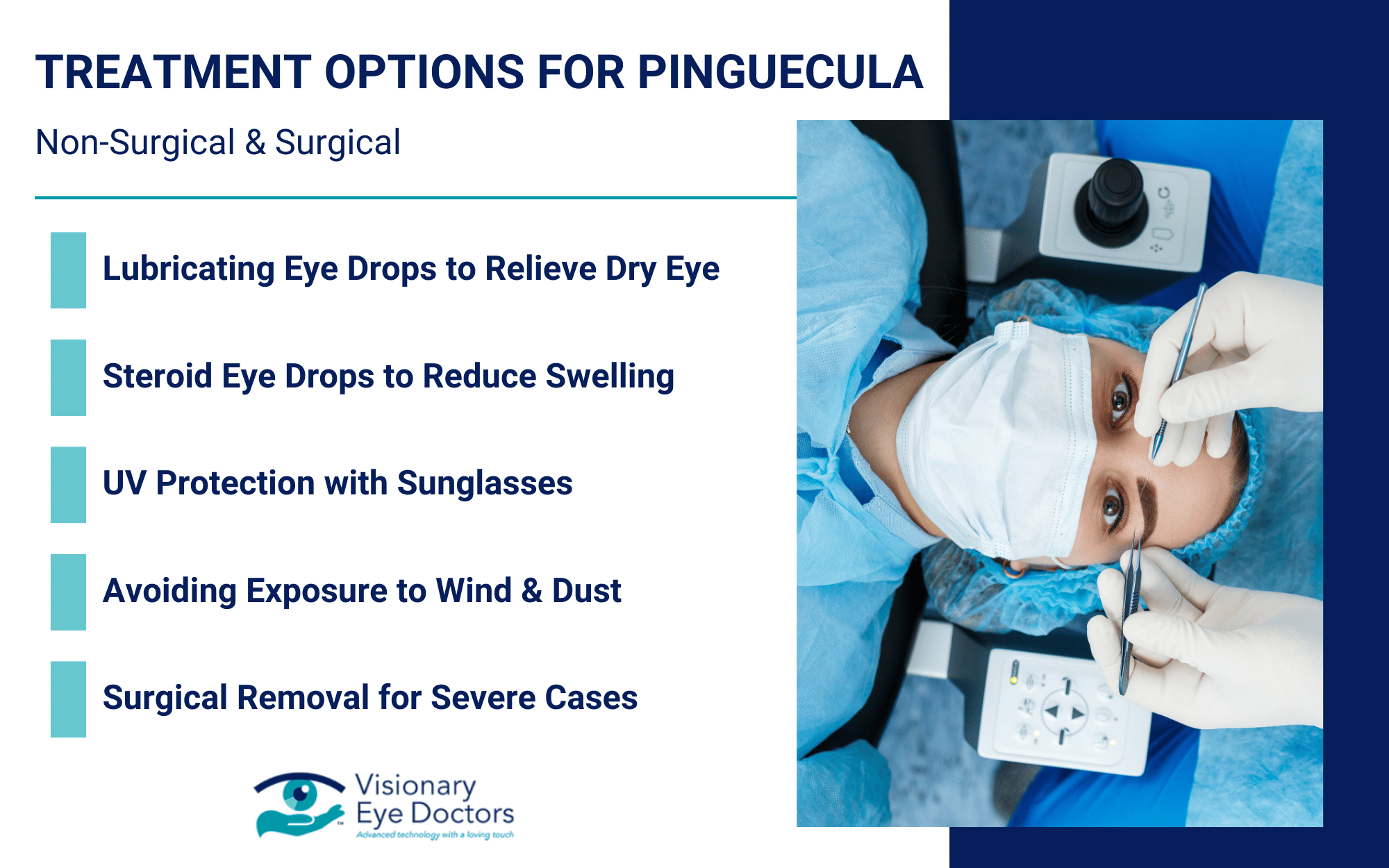
Non-Surgical Treatments
For early-stage diabetic retinopathy, treatment focuses on stabilizing blood sugar levels, blood pressure, and cholesterol to reduce stress on the retinal blood vessels.
- Anti-VEGF Injections are injected directly into the eye to block the growth of abnormal blood vessels and help reduce macular edema, potentially stabilizing or improving vision in some patients.
- Corticosteroid Injections are anti-inflammatory agents that may be used to reduce swelling and inflammation in the retina, especially for those with persistent diabetic macular edema.
Surgical Options
When diabetic retinopathy reaches the advanced stage, surgery may be necessary.
- Laser Therapy
- Focal/Grid Laser Treatment targets specific areas of the retina and seals leaking blood vessels to reduce fluid buildup and swelling.
- Panretinal Photocoagulation targets a wider area of the retina, preventing bleeding and reducing the risk of retinal detachment.

Protecting Your Vision with Expert Eye Care
Managing diabetic retinopathy requires consistent care and early intervention. While treatments can help slow progression and prevent vision loss, the best way to protect your eyesight is through proactive management and getting regular eye exams at the eye doctor.
Why Ongoing Eye Care Matters
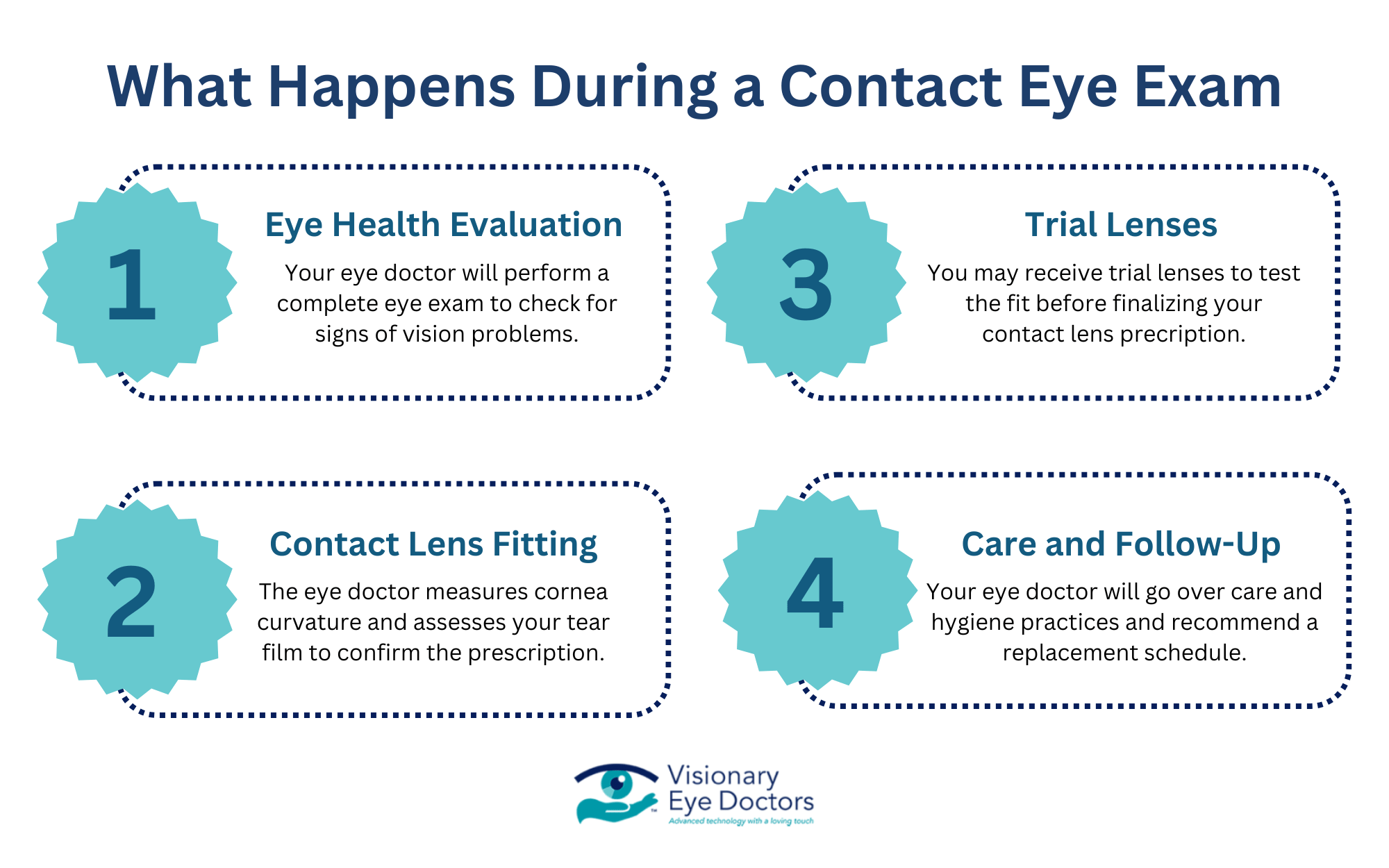
Diabetic retinopathy often develops without noticeable symptoms, making regular eye exams essential. A comprehensive eye exam, including optical coherence tomography (OCT) and dilated retinal imaging, can detect changes in the retina before vision is affected.
How Visionary Eye Doctors Can Help
At Visionary Eye Doctors in the Washington, DC, and Maryland area, our team specializes in diagnosing, monitoring, and treating diabetic retinopathy using advanced technology and personalized care. We provide:
- Comprehensive eye exams to detect early signs of retinal changes
- Expert treatment options, including focal and scatter laser treatment
- Guidance on managing blood sugar, blood pressure, and lifestyle habits to help protect your vision
Take the Next Step in Protecting Your Vision
Don’t wait for noticeable symptoms to appear. Schedule a comprehensive eye exam at Visionary Eye Doctors today to take control of your eye health and prevent any further damage to your vision.