Understanding the Differences Between Cataracts and Glaucoma
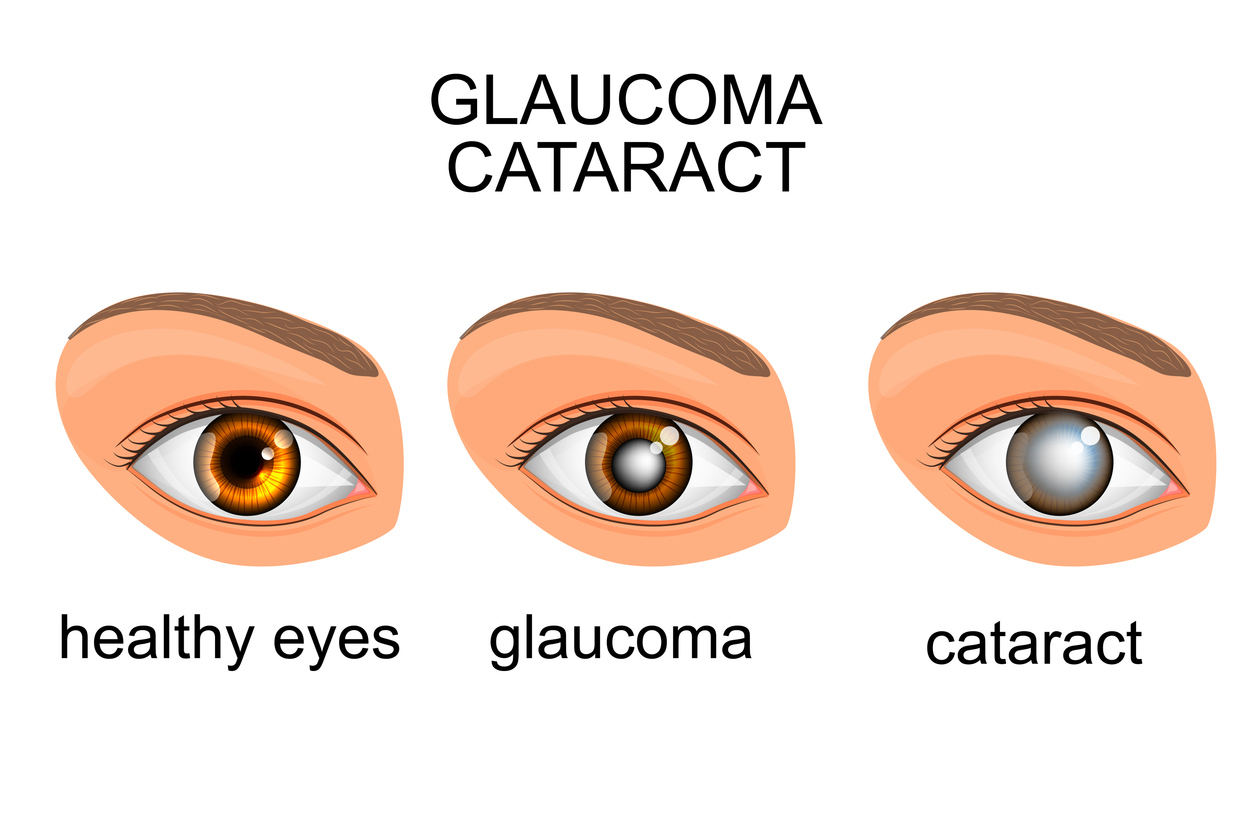
When it comes to understanding the differences between cataracts and glaucoma, knowing the basics can provide helpful insight into each condition’s impact on eye health. Both are common eye conditions but differ significantly in causes, symptoms, and treatment options.
In brief:
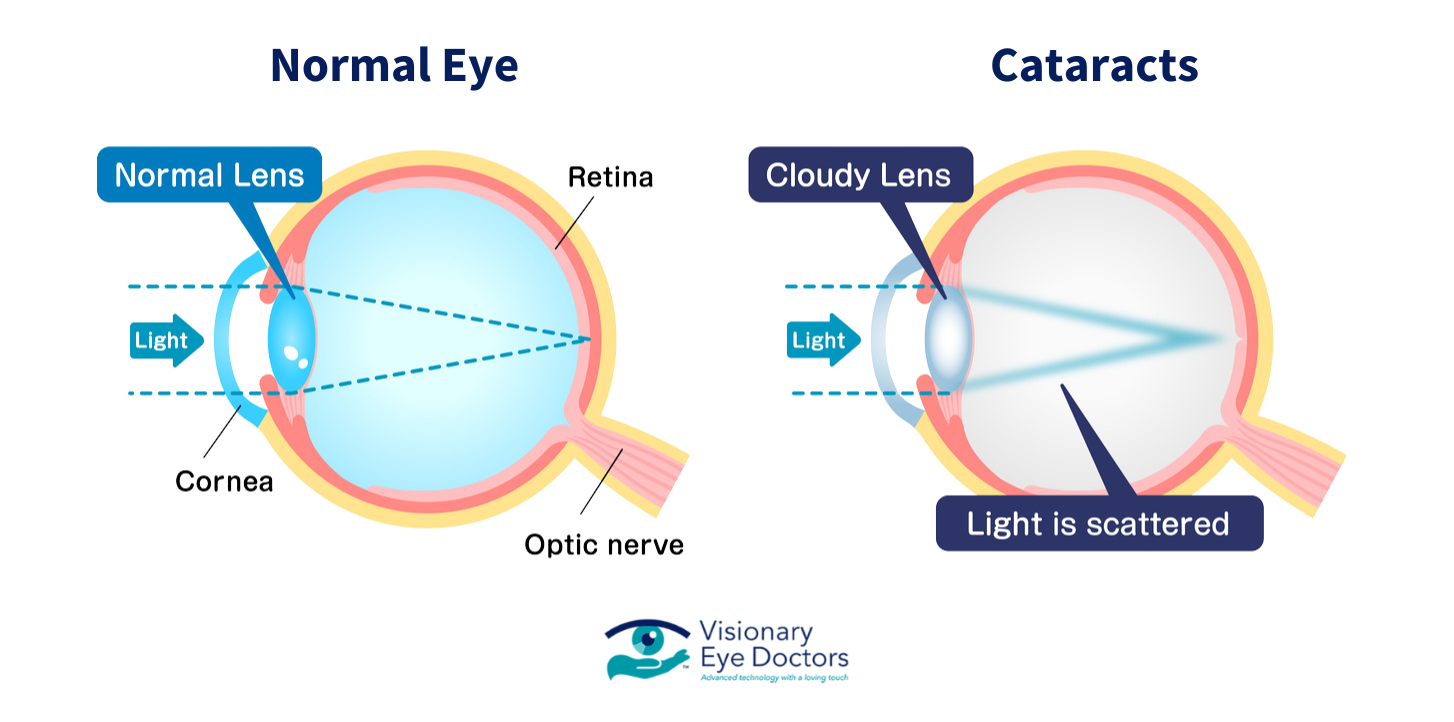
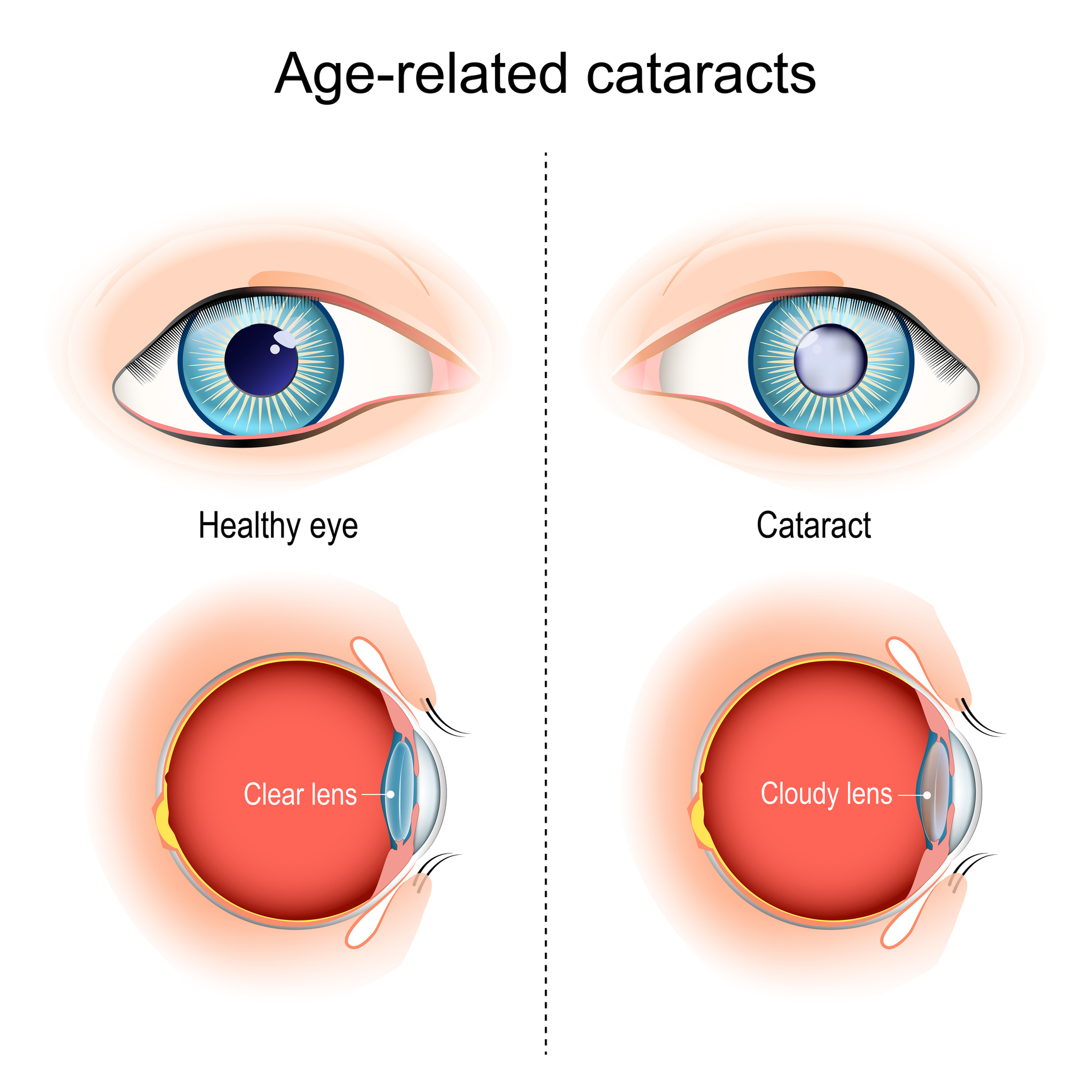
- Cataracts result from a clouding of the eye’s natural lens, which can lead to blurry vision, sensitivity to light, and a gradual decline in visual clarity. Cataracts usually develop as a part of aging, affecting vision over time but often treatable with cataract surgery to restore clear vision.
- Glaucoma, on the other hand, is an eye disease primarily affecting the optic nerve, often due to increased intraocular pressure. This pressure can lead to gradual vision loss, particularly peripheral vision, and, if left untreated, can result in irreversible blindness. Unlike cataracts, glaucoma’s damage is often permanent, making early detection essential.
While cataracts affect the eye’s lens, causing visible cloudiness, glaucoma is known as the “silent thief of sight” due to its typically unnoticed progression. For those interested in more in-depth information on each condition and ways to manage or treat them, we’ll explore further below.
Cataracts: Causes, Symptoms, and Treatment Options
Cataracts are a common eye condition that results in a gradual clouding of the eye’s natural lens, leading to vision impairment over time. While cataracts are often associated with aging, they can also develop due to factors like excessive UV exposure, diabetes, smoking, and certain medications. By understanding the primary causes and symptoms, you can take steps toward early detection and treatment.
Causes:
Cataracts are largely age-related, typically forming in adults over the age of 60. However, additional risk factors, such as long-term UV exposure, a history of smoking, diabetes, and previous eye injuries, can increase the likelihood of developing cataracts. Over time, these factors contribute to protein buildup on the eye’s lens, creating a cloudy effect that blocks light from reaching the retina.
Symptoms:
The cataract symptoms often start subtly, with many people experiencing a gradual worsening of their vision. Common symptoms include:
- Cloudy or Blurry Vision: Vision may become hazy, as if looking through a fogged-up window.
- Yellowing of Colors: Colors may appear faded or less vibrant.
- Increased Sensitivity to Light and Glare: Bright lights, especially at night, can cause discomfort or halos around light sources.
- Difficulty Seeing at Night: Night driving or seeing in low-light conditions becomes challenging.
- Frequent Prescription Changes: You might notice that your glasses or contact prescription needs frequent updating.
Treatment Options:
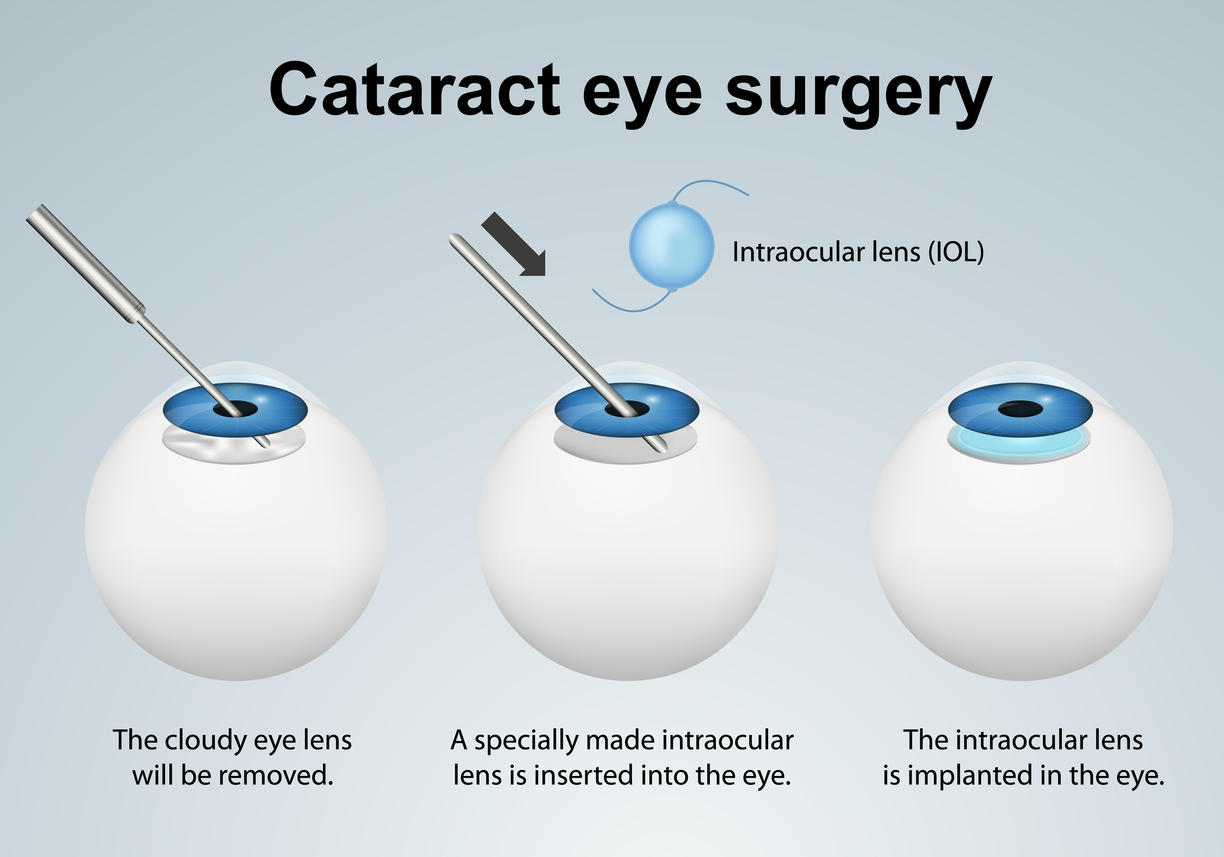
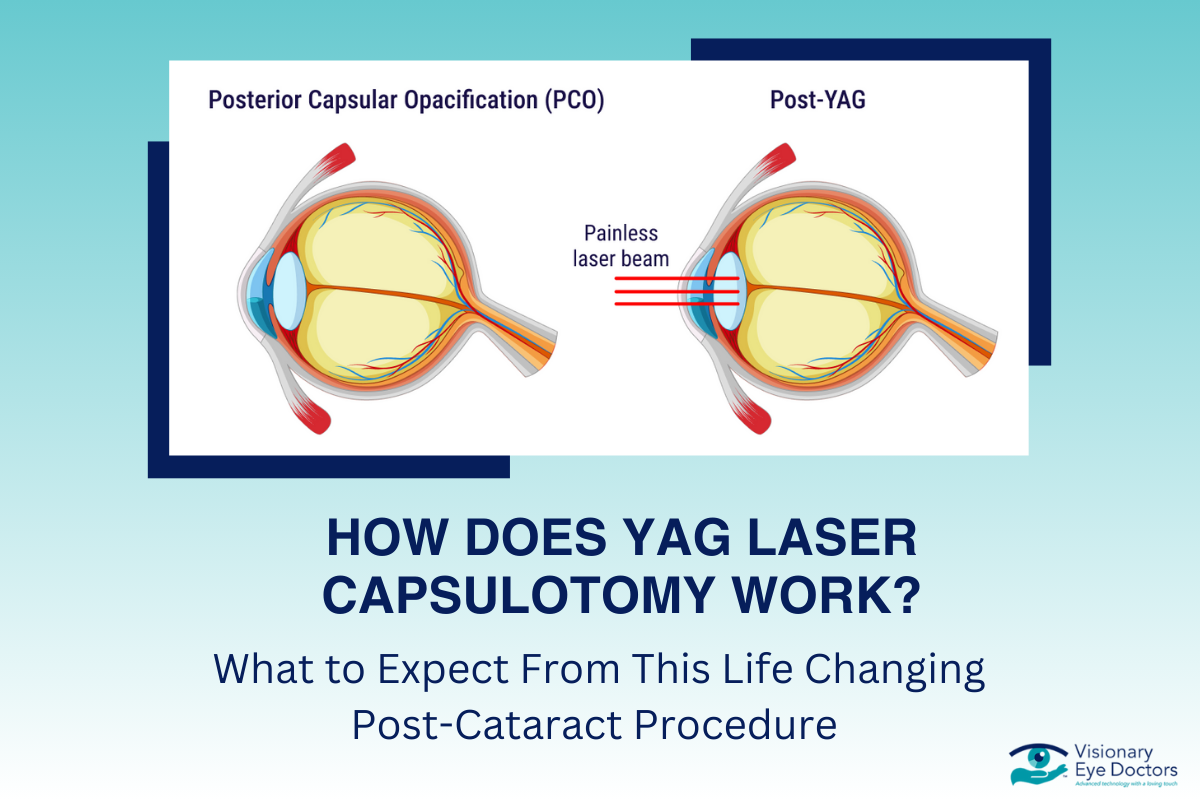
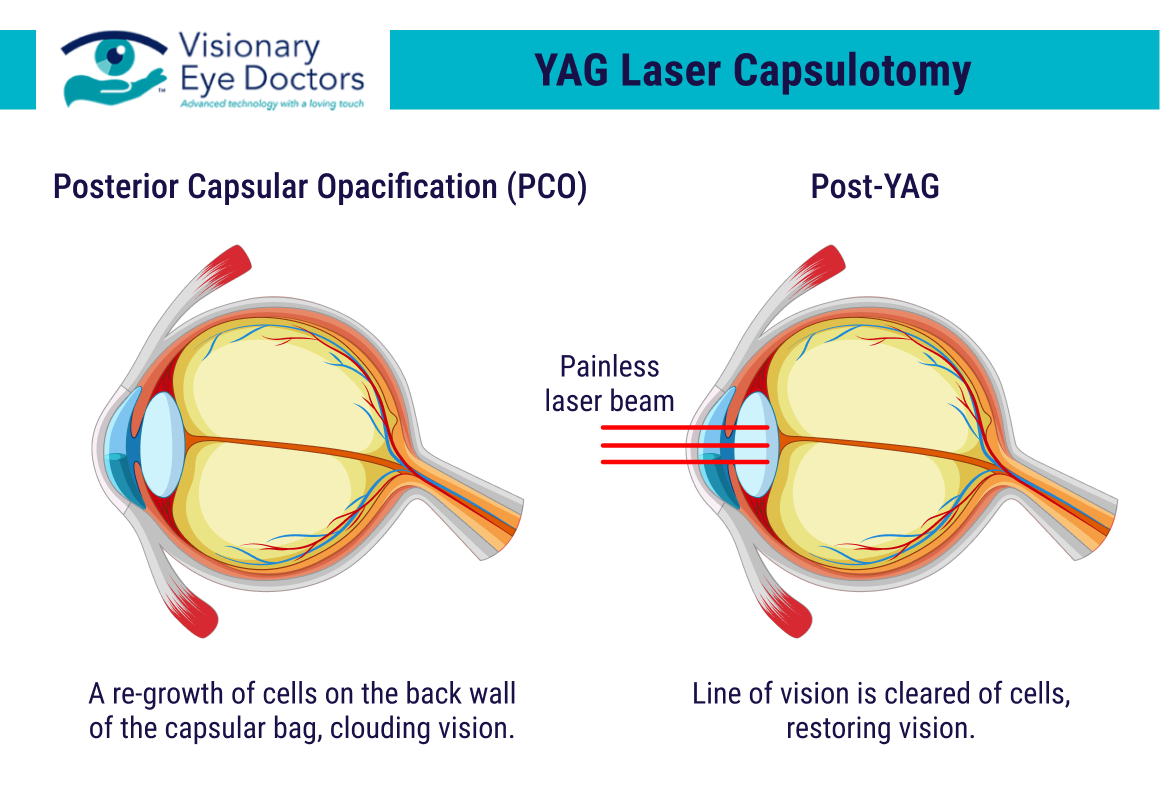
The only definitive treatment for cataracts is surgery, specifically cataract removal and lens replacement surgery. In this procedure, the clouded lens is removed and replaced with an intraocular lens, restoring clear vision. This surgery is safe and effective, offering options for different types of lenses that can improve both near and distant vision. Post-surgery, many people experience significant improvement in their vision and may even reduce their dependency on corrective lenses.
Cataracts are highly treatable, and surgery offers a long-term solution for clear vision. Early detection through regular eye exams can make a significant difference, allowing for timely intervention and improved visual outcomes.
Glaucoma: Causes, Symptoms, and Treatment Options
Glaucoma is a serious eye disease that damages the optic nerve, often as a result of increased intraocular pressure. Unlike cataracts, glaucoma’s damage is usually irreversible, which is why early detection and regular monitoring are essential for preventing permanent vision loss. Several types of glaucoma exist, each with distinct characteristics and treatment needs.
Causes and Risk Factors:
Glaucoma is generally caused by high pressure within the eye, known as intraocular pressure, which can damage the optic nerve over time. Key risk factors include age (especially in adults over 60), family history of glaucoma, certain medical conditions like diabetes, and high blood pressure. The disease is more common in African American, Hispanic, and Asian populations, making regular screenings vital for early detection.
Types of Glaucoma:
- Open-Angle Glaucoma: This is the most common type, where eye pressure builds up gradually, leading to slow vision loss. Often, there are no symptoms until significant damage has occurred.
- Angle-Closure Glaucoma: This type occurs when the drainage angle between the iris and cornea closes, causing a sudden spike in eye pressure. Symptoms can include severe eye pain, nausea, blurred vision, and seeing halos around lights.
- Secondary Glaucoma: This can occur due to another eye condition, injury, or as a side effect of certain medications.
Symptoms:
Glaucoma is known as the “silent thief of sight” because it often presents no noticeable symptoms in its early stages. As it progresses, people may experience:
- Loss of Peripheral Vision: Vision loss typically starts at the edges, causing tunnel vision.
- Eye Pain and Redness (in cases of angle-closure glaucoma): Symptoms may come on suddenly and be accompanied by headaches or nausea.
- Blurred Vision and Halos Around Lights: Particularly noticeable in low-light conditions.
Treatment Options:
Glaucoma treatment focuses on lowering intraocular pressure to slow down or prevent optic nerve damage. Treatment options include:
- Eye Drops: Often the first line of treatment, these medications help reduce eye pressure.
- Laser Treatment: Laser surgery can improve fluid drainage in the eye, effectively lowering pressure.
- Glaucoma Surgery: In more advanced cases, surgical procedures are available to create a new drainage pathway in the eye, helping to maintain normal pressure levels
- Minimally Invasive Glaucoma Surgery (MIGS): A newer surgical option that uses tiny incisions and devices to improve fluid drainage, lowering eye pressure with a faster recovery time compared to traditional surgery.
While there is no cure for glaucoma, these treatment options can help manage the disease and preserve remaining vision. For glaucoma patients, regular eye exams and early intervention are crucial in preventing further vision impairment and maintaining quality of life.
Key Differences Between Cataracts and Glaucoma
Understanding the key differences between cataracts and glaucoma can help individuals take proactive steps to manage their eye health effectively. Although both conditions affect vision, they differ significantly in how they develop, impact the eye, and respond to treatment. Here’s a closer look at what sets them apart:
Vision Impact:
Cataracts:
Primarily affect the eye’s lens, leading to cloudy or blurry vision that worsens over time. The vision changes from cataracts are typically gradual and can cause difficulty with tasks like reading, recognizing faces, or seeing in low light.
Glaucoma:
Damages the optic nerve, often resulting in a slow loss of peripheral vision, which can eventually lead to tunnel vision. Unlike cataracts, glaucoma’s impact on vision is usually irreversible and can lead to permanent vision loss if not managed early.
Progression and Detection:
Cataracts:
Develop visibly and progressively, making it easier to recognize symptoms like cloudiness, color fading, and increased glare sensitivity. They can often be detected during routine eye exams and treated with cataract surgery for a permanent solution.
Glaucoma:
Known as the “silent thief of sight,” glaucoma often progresses without symptoms, especially in the early stages. Vision loss from glaucoma is generally not noticeable until the disease has significantly advanced, underscoring the importance of regular eye exams, especially for those at higher risk.
Treatment Differences:
Cataracts:
Treatment involves cataract removal surgery, where the cloudy lens is replaced with an artificial intraocular lens, providing a long-term solution for clear vision. Most patients experience significant improvements in vision post-surgery.
Glaucoma:
Treatments focus on managing and lowering eye pressure to prevent further optic nerve damage. Options include eye drops, laser surgery, and, in more severe cases, surgical procedures. Glaucoma treatment can slow progression but cannot reverse existing vision loss.
In summary, cataracts can be treated successfully with surgery to restore vision, while glaucoma requires ongoing management to prevent further damage. Regular eye exams and early detection are crucial for both conditions, helping preserve vision and improve quality of life.
Choosing the Right Care for Cataracts or Glaucoma: How Visionary Eye Doctors Can Help

When it comes to managing cataracts or glaucoma, selecting a trusted, experienced eye care provider is essential to achieve the best possible outcomes. At Visionary Eye Doctors, we recognize the unique needs each condition presents and provide individualized care to help restore and protect your vision.
Early detection and comprehensive eye exams are crucial to managing both cataracts and glaucoma. For cataracts, regular exams allow for prompt diagnosis and timely intervention, often leading to significantly improved vision. For glaucoma, early diagnosis is even more critical, as the disease’s progression can be slowed, preserving your vision and overall quality of life. Our team at Visionary Eye Doctors is dedicated to creating proactive treatment plans that prioritize your long-term eye health.
For those with cataracts, Visionary Eye Doctors offers cutting-edge cataract removal surgery using advanced surgical technology and premium intraocular lenses. Our skilled surgeons aim to restore clear vision through a range of lens options, often reducing or eliminating the need for glasses for both near and far vision. We understand that each patient’s vision needs are different, and we work closely with you to select the best surgical approach and lens type for your lifestyle and preferences.
Glaucoma patients also benefit from a full spectrum of treatment options, including prescription eye drops, laser treatments, and advanced surgical procedures. Our approach centers on reducing intraocular pressure to prevent further optic nerve damage and maintain your vision. Throughout your treatment journey, our compassionate team is committed to supporting you every step of the way, offering the latest in glaucoma management to achieve optimal results.
Visionary Eye Doctors is dedicated to providing high-quality, personalized care to patients in Washington, D.C., and surrounding areas. With a team of board-certified surgeons and a state-of-the-art facility, we strive to make every experience as comfortable, reassuring, and effective as possible. Take the next step in protecting or restoring your vision by scheduling a consultation with Visionary Eye Doctors today, and let us help you see a brighter future.\









 With age, sometimes, comes vision loss. Issues like blurred sight, cloudy vision, and light sensitivity can interfere with your daily activities and significantly affect your quality of life. These are often the first signs of
With age, sometimes, comes vision loss. Issues like blurred sight, cloudy vision, and light sensitivity can interfere with your daily activities and significantly affect your quality of life. These are often the first signs of 

 Cutting-edge Technology:
Cutting-edge Technology: 


 Cataract Surgery Overview
Cataract Surgery Overview