What You Need to Know About Glaucoma Awareness Month
January is National Glaucoma Awareness Month, a time dedicated to educating people about glaucoma, its risk factors, and the importance of early detection. As one of the leading causes of irreversible vision loss in the United States, glaucoma affects millions worldwide – yet many don’t realize they have it until significant damage has already occurred.
Why Awareness Matters
Glaucoma often has no noticeable symptoms in the early stages, making routine eye exams a critical part of early detection. Raising awareness for this eye condition can help people prevent themselves from permanent vision loss by promoting timely treatment and proactive eye care.
A Deep Dive into Glaucoma
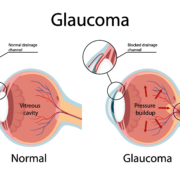
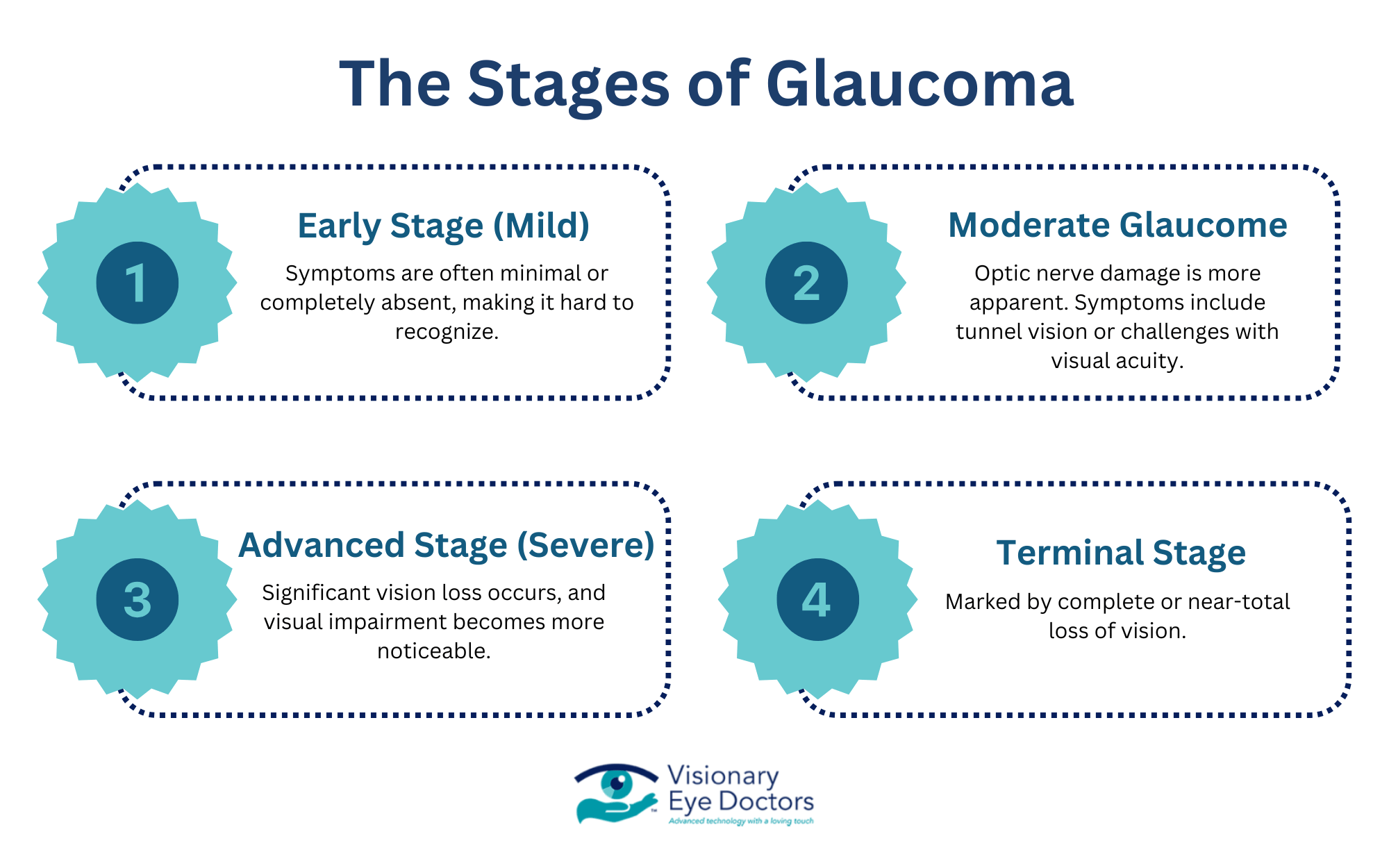
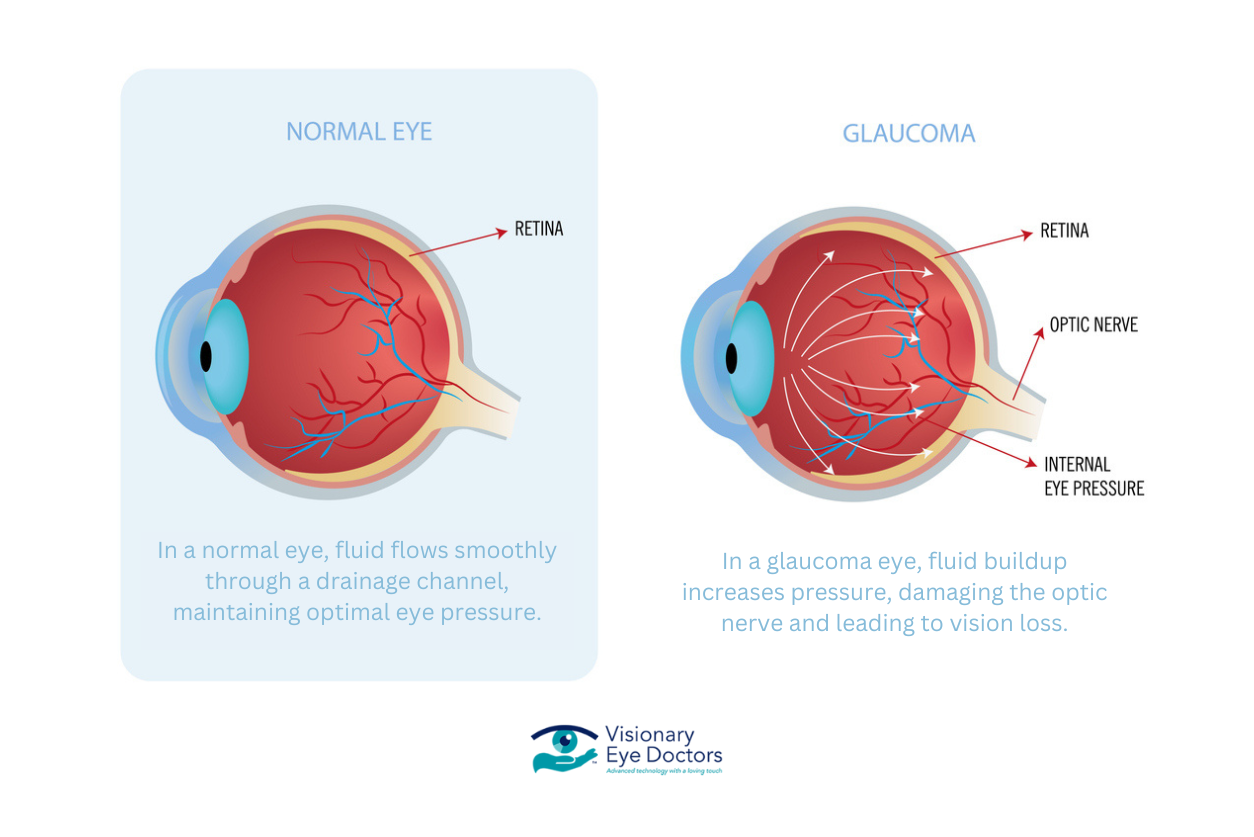
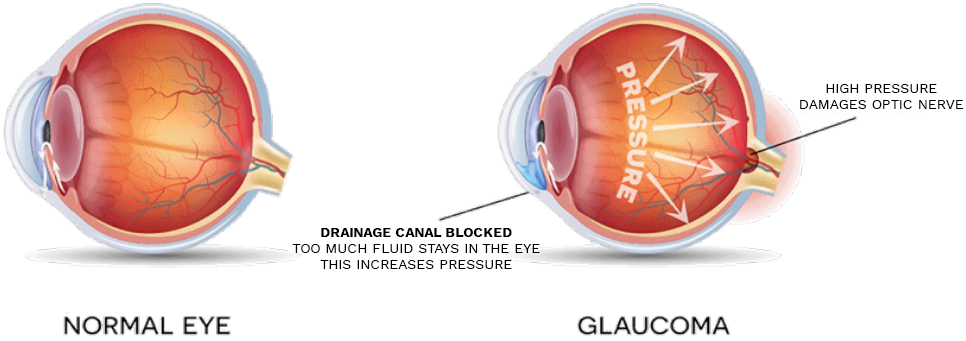
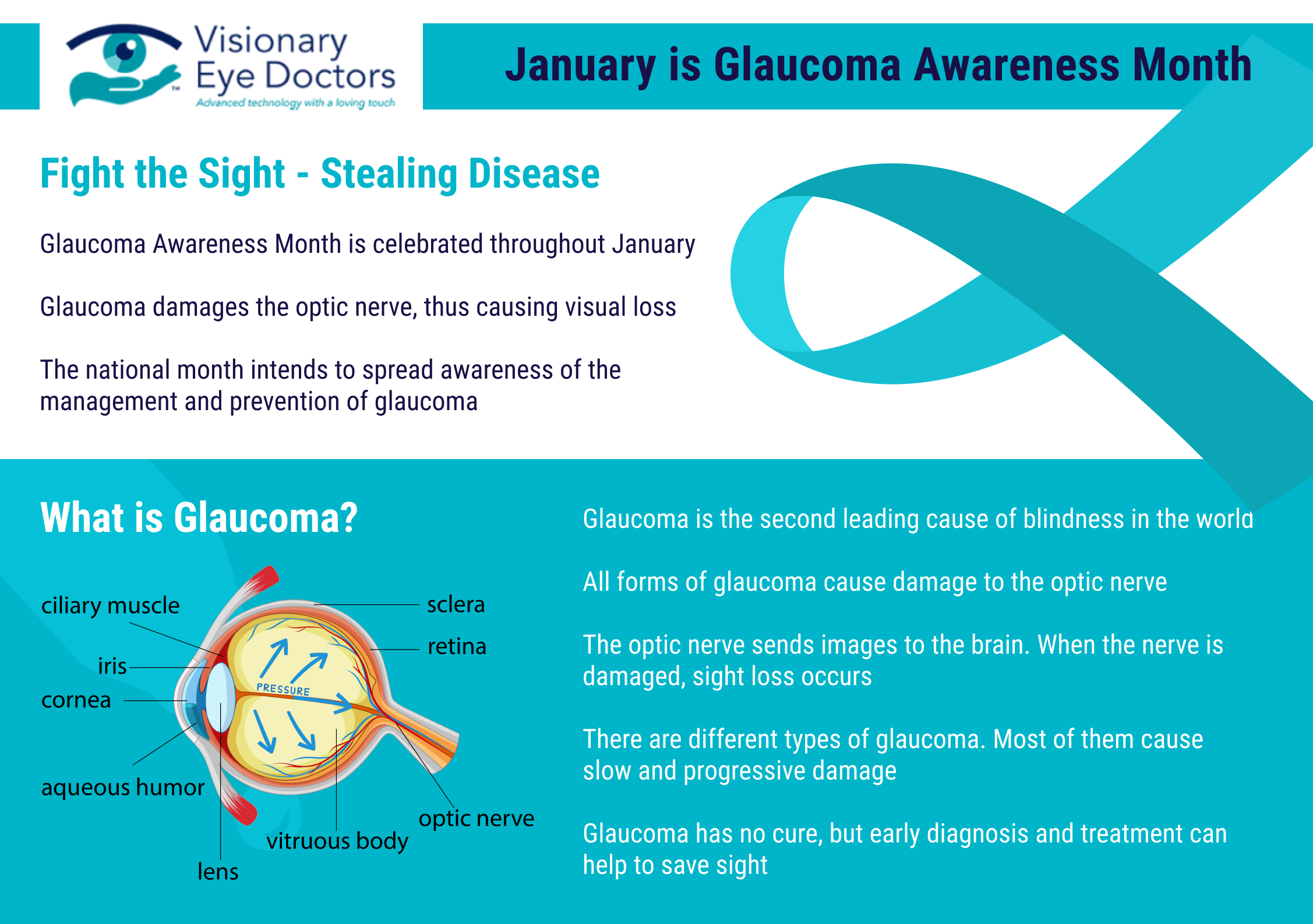
Definition: Glaucoma is a group of progressive eye diseases that damage the optic nerve, leading to vision loss and, if left untreated, blindness. While most cases are associated with high intraocular pressure (IOP), some types can develop even when eye pressure is within a normal range.
How Glaucoma Affects Vision
The optic nerve is responsible for transmitting visual information from the eye to the brain. When glaucoma damages this nerve, it disrupts vision – typically starting with small blind spots in peripheral vision. Over time, optic nerve damage can progress, leading to significant vision impairment or complete blindness.
Types of Glaucoma
Open-Angle Glaucoma
- The most common type – develops when the eye’s drainage system becomes blocked.
- Progresses slowly and often goes unnoticed until vision loss occurs.
Angle-Closure Glaucoma
- A sudden and severe blockage in the eye’s drainage canals causes a rapid rise in eye pressure.
- Symptoms are severe eye pain, blurred vision, nausea, and headaches.
Secondary Glaucoma
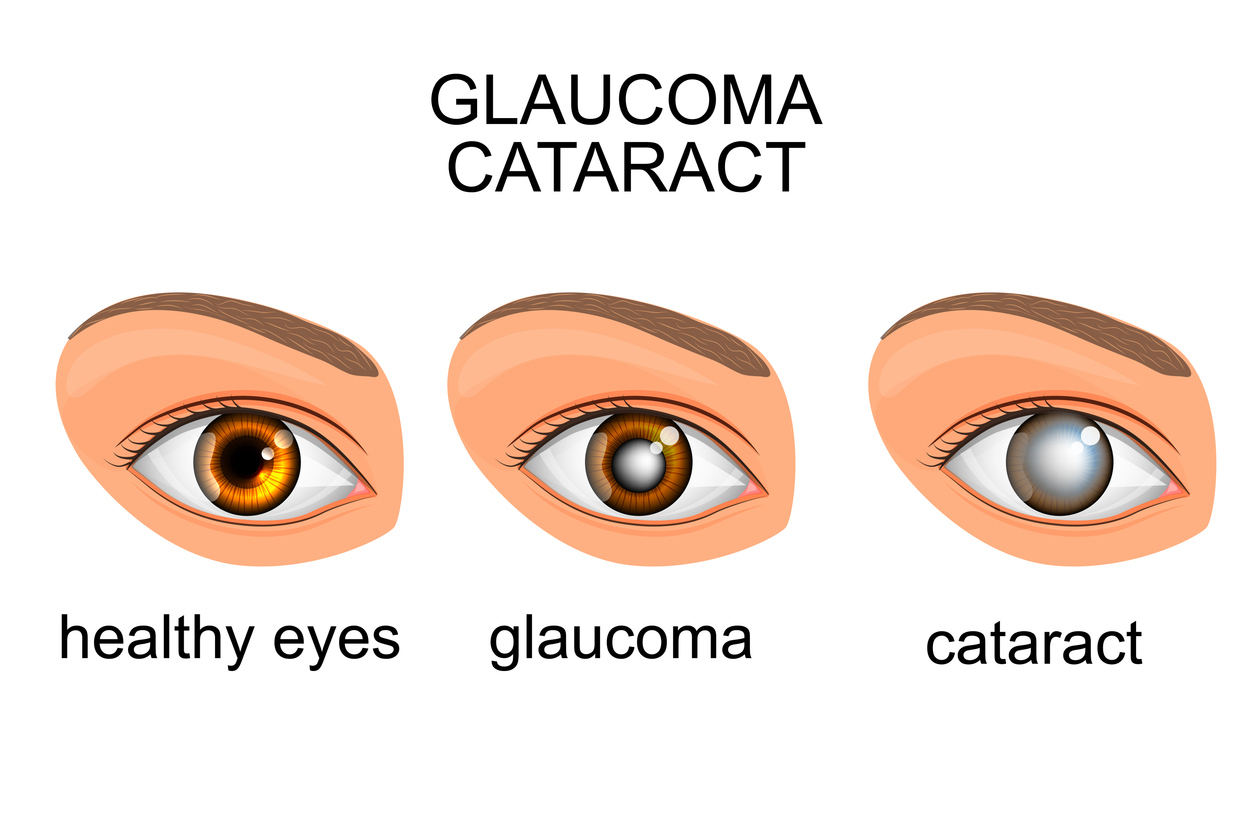
- Caused by underlying conditions like diabetic retinopathy, cataracts, or eye trauma.
- Treating the underlying cause can help manage this type of glaucoma.
Congenital Glaucoma
- Rare and present at birth – occurs due to abnormal eye development in newborns.
- Early signs include excessive tearing, light sensitivity, and an enlarged eye.
Who is Most at Risk for Glaucoma?
Certain people have a higher likelihood of developing glaucoma due to genetic, medical, and lifestyle factors. Those at greater risk include:
- African Americans and Hispanics, especially at a younger age
- Individuals over 40 years old
- People with long-term steroid use
- People with a family history of glaucoma
- Individuals with high intraocular pressure (IOP)
- Those with chronic conditions – diabetes, heart disease, or extreme nearsightedness
- People with past eye injuries, thin corneas, or drainage problems
Early Symptoms and Warning Signs
Many people are unaware of glaucoma until significant vision loss has occurred. Some warning signs that may indicate glaucoma include:
- Blurred vision
- Frequent headaches
- Eye strain
- Halos around lights
- Difficulty adjusting to low light
- Patchy blind spots in side vision
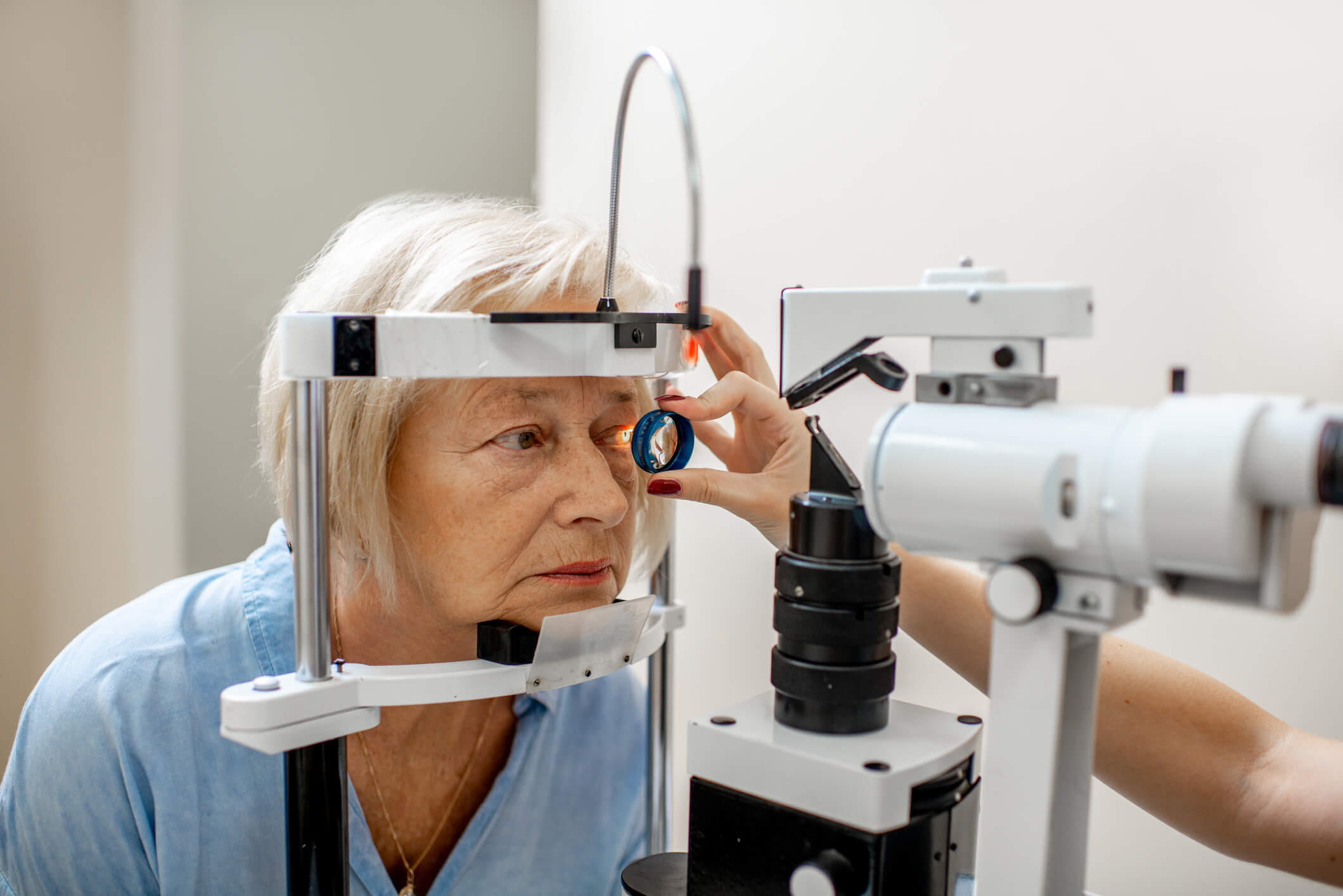
Importance of Regular Eye Exams
A comprehensive eye exam is the most reliable way to detect glaucoma early. Since these symptoms often go unnoticed until irreversible damage has occurred, routine screenings are crucial – especially for those at higher risk.
The National Eye Institute recommends annual glaucoma screenings for individuals with risk factors to ensure early diagnosis and treatment.

Glaucoma Prevention and Treatment Options
While glaucoma cannot be cured, early diagnosis and proactive care can help prevent significant vision loss. Steps to reduce risk and slow progression include:
- Regular comprehensive eye exams – the best way to catch glaucoma early and prevent permanent damage. Get regular eye exams:
- Before age 40 – every 2 or 3 years
- From age 40 to 54 – every 1 to 3 years
- From age 55 to 64 – every 1 to 2 years
- After age 65 – every 6 to 12 months
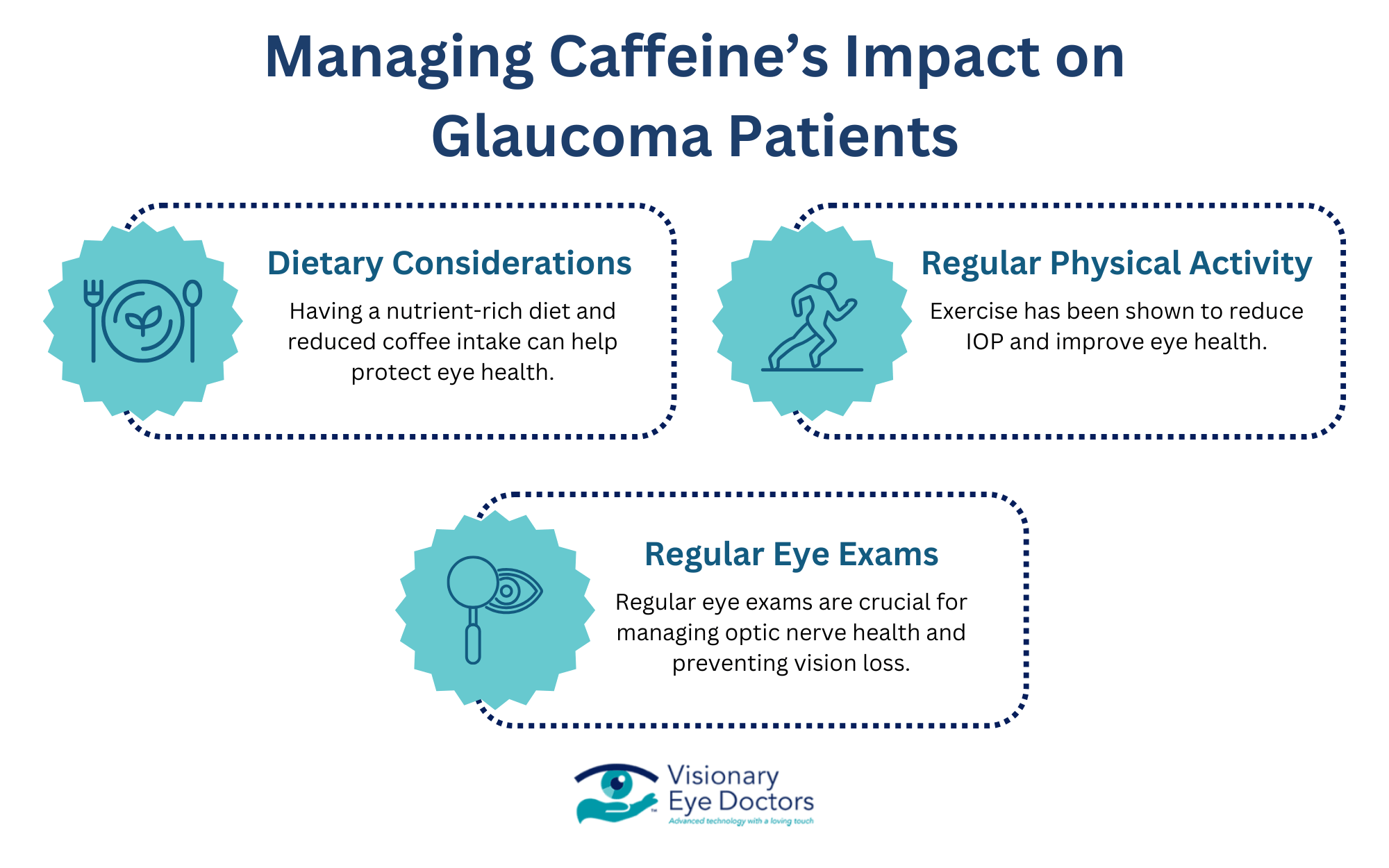
- Maintaining a healthy lifestyle – regular exercise, a balanced diet, and hydration can help lower intraocular pressure.
- Managing underlying health conditions – controlling blood pressure and diabetes supports overall eye health.
Glaucoma Treatment Options
Although glaucoma damage is irreversible, appropriate treatment can slow or prevent further vision loss. Treatment plans are tailored to each patient’s needs and may include:
Prescription Medications
- Prescription eye drops that help maintain eye pressure at a healthy level. They measure changes in the peripheral visual field, helping to improve fluid drainage or decrease fluid production.
Laser Treatments for Glaucoma
- Selective Laser Trabeculoplasty uses short pulses to target specific cells in the eye’s drainage system and stimulate improved function. This procedure can slow or stop the risk of disease progression.
Surgical Procedures
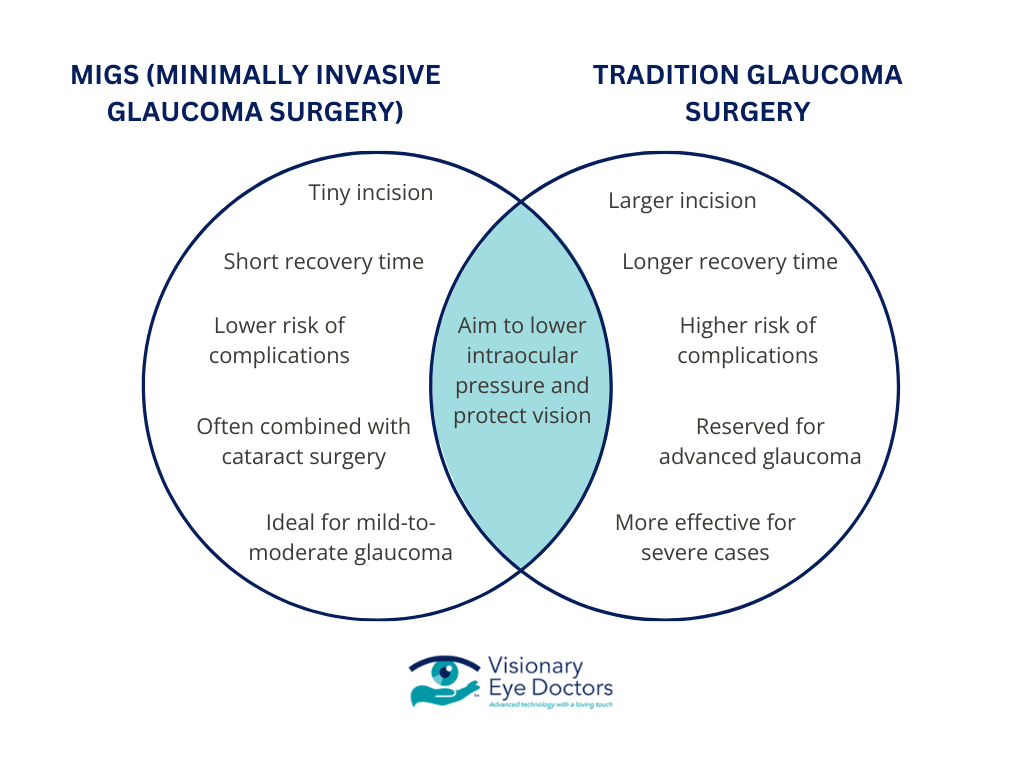
- Minimally Invasive Glaucoma Surgery (MIGS) – A less invasive option that improves drainage. Widely accepted as one of the most successful techniques for mild-to-moderate glaucoma.
- Trabeculectomy – A traditional surgery that creates a new drainage pathway to reduce pressure. It’s performed when eye drops or laser surgery aren’t effective.
Lifestyle Adjustments
- Managing blood pressure and diabetes, maintaining a nutrient-rich diet, and avoiding habits that increase eye pressure (such as smoking) can support long-term eye health.

Visionary Eye Doctors: Leading the Way in Glaucoma Care
At Visionary Eye Doctors, we combine expertise, advanced technology, and personalized care to help glaucoma patients manage their eye conditions effectively. Our glaucoma specialists provide cutting-edge diagnostics and customized treatment plans to protect and preserve vision.
Our Trusted Surgeons
Dr. Reena A. Garg is a Board-Certified & Fellowship-trained Ophthalmologist. She specializes in glaucoma treatment – including MIGS (minimally invasive glaucoma surgeries) – and cataract surgery.
Dr. Georgina Medina, M.D., specializes in Glaucoma, Cataract, and Comprehensive Ophthalmology. With extensive training from Emory Eye Center, she brings expertise in managing and treating glaucoma and related conditions.
Our Comprehensive Approach to Glaucoma Treatment
Our ophthalmologists are committed to early detection and proactive management, offering:
- Advanced Imaging Technology – Detects glaucoma in its earliest stages before significant vision loss occurs.
- Personalized Treatment Plans – Tailored to each patient’s unique risk factors and disease progression.
- Access to the Latest Glaucoma Therapies – Including prescription medications, laser treatments, and minimally invasive surgical procedures.
Protect Your Vision, Spread Awareness
Glaucoma Awareness Month is a time to educate, take action, and protect your vision. Since glaucoma often has no early symptoms, regular eye exams are the key to preventing permanent vision loss.
If you are at risk, don’t wait – prioritize your eye health today. Schedule a comprehensive eye exam with our glaucoma specialists today!
Resources:
https://glaucoma.org/articles/january-is-glaucoma-awareness-month
https://glaucoma.org/treatment/laser/slt














 Meet Our Glaucoma Specialists
Meet Our Glaucoma Specialists